IBS Support: How the Four R Program Can Help
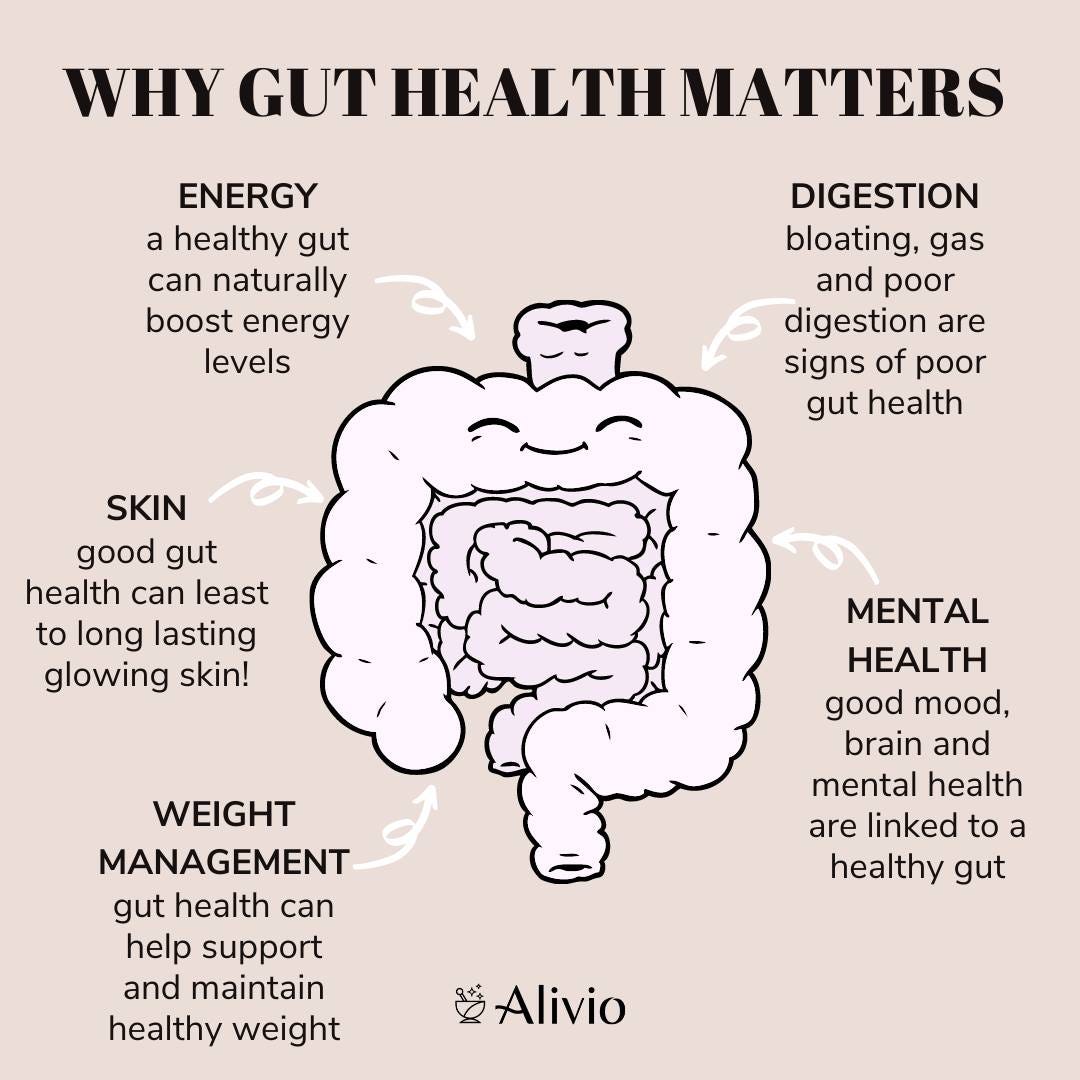
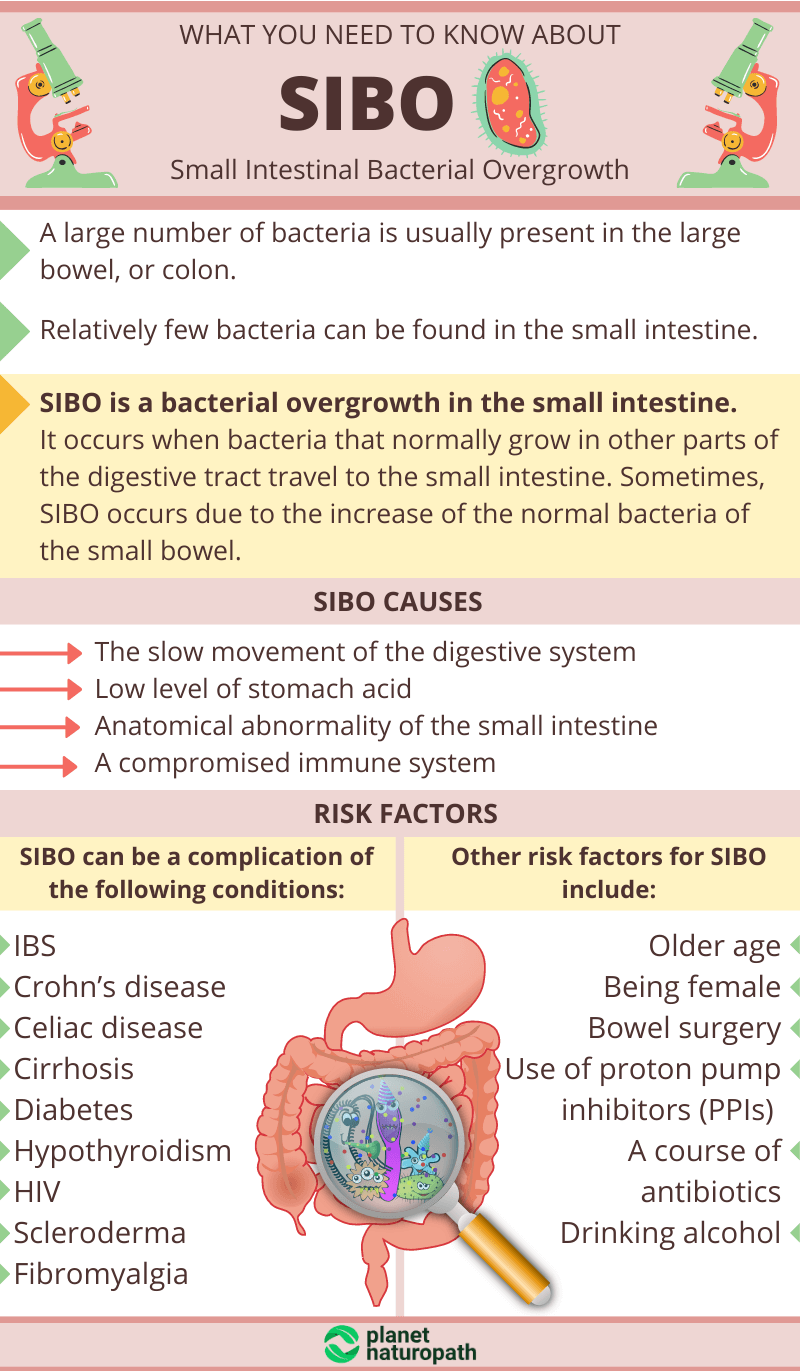
Irritable bowel syndrome (IBS) is a frequently diagnosed gastrointestinal disorder accounting for an excess of 2 million family physician visits in 2002 within the United States.1 Furthermore, IBS is a multifactorial and complex disorder often characterized by abdominal pain, discomfort, altered bowel habits, as well as bloating and gas.1(261) The pathophysiology of IBS can include heightened visceral sensitivity (low threshold for gastrointestinal-related pain), increased intestinal permeability (covered previously in this author’s posts), and small intestinal bacterial overgrowth (SIBO).1(263-264) Having briefly considered IBS, the following will explore tests identifying its underlying drivers, and protocols/solutions for the same.
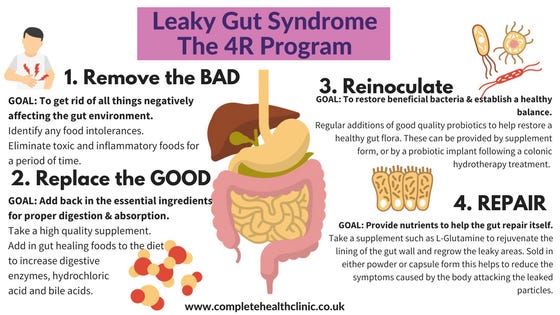
Once IBS has been diagnosed (please see this author’s previous posts), Lord et al2 outlined a protocol which provides a pragmatic and systematic approach in addressing the underlying pathophysiology of said condition; such a protocol is known as the Four R Program (FRP).2(453) FRP is characterized by 4 phases: phase 1-removing allergenic foods and microbial overgrowth using bacteriostatic (slows bacterial reproduction)/mycostatic (slows fungal reproduction) agents, phase 2-replacing digestive enzymes, phase 3-reinoculating with favorable microbes, and phase 4-repairing gastrointestinal tissue and immune system integrity.2(454) The following will consider FRP steps in greater detail, as well as tests indicating their requirement.
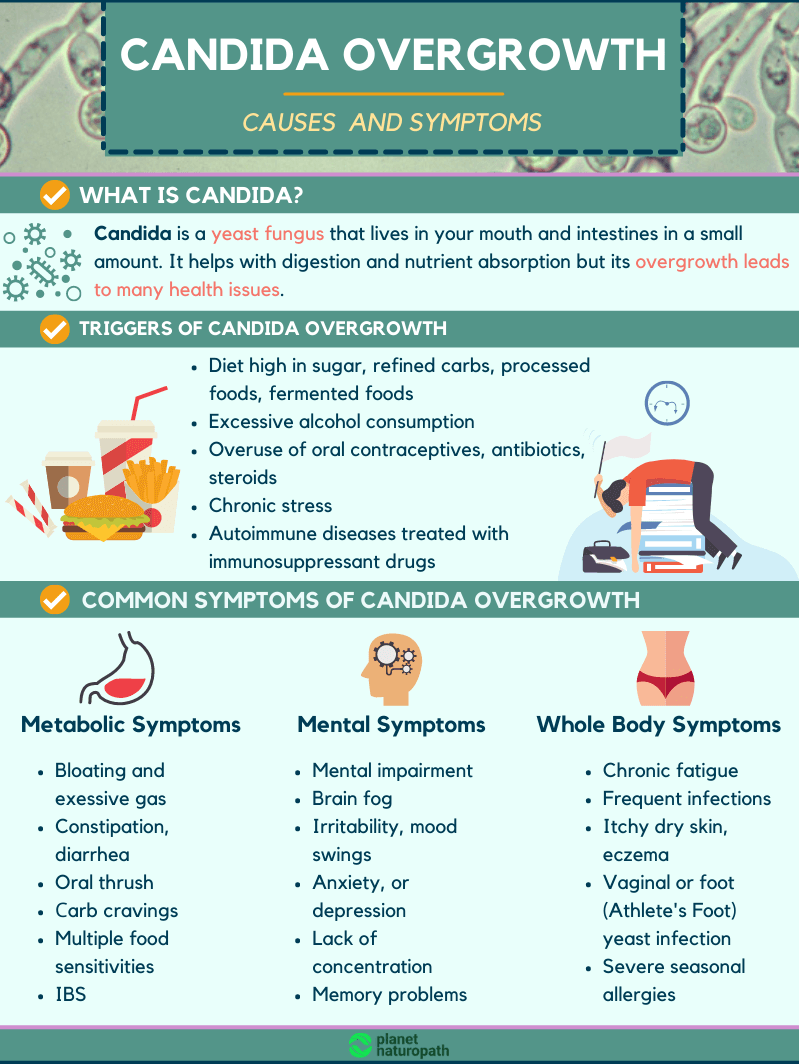
Several tests can indicate dysbiosis; an intestinal condition where the microbiota produces harmful effects through quantitative and qualitative changes in the intestinal flora; alterations in microbial metabolic activity; and changes in microbial distribution.3 When considering the first step in FRP (remove), consideration of foods which could cause aberrations in intestinal function is critical. If, for example, food allergy tests identified highly reactive foods (which drive IgG antibodies) such as yogurt/cheese/casein/mozzarella cheese, removal of the same would be a logical first step. Once removal of allergens is completed, removal and control of non-beneficial/over-populated microbes is the second half of phase 1 FRP.
Tests that identify microbial overgrowth can include organic acid markers such as hippurate and indican as well as DNA testing, by analysis of polymerase chain reactions (PCR), to detect Bacteroides vulgaatus, Barnsiella spp., Provetella spp., Faecalibacterium prausnitzii, Pseudoflavonifractor spp., and Methanobrevibacter smithii.2(448) High hippurate can be indicative of detoxification challenges and/or dysbiosis while high indican concentrations often denotes bacterial overgrowth in the upper bowel.2(376,384) The high concentrations of Bacteroides vulgaatus, Barnsiella spp., Provetella spp., Faecalibacterium prausnitzii, Pseudoflavonifractor spp., and Methanobrevibacter smithii can be problematic. For example, overpopulation of Bacteroides vulgaatus has been associated with Crohn’s disease and ulcerative colitis while overpopulation of Methanobrevibacter smithii has been associated with excessive production of methane gas, bloating, and constipation.5
If organic acid markers and PCR testing indicates overgrowth of bacterial/fungal microbes, general recommendations can include a high fiber diet (to improve gut motility), but one low in fermentable fiber carbohydrates, especially if PCR tests indicate Methanobrevibacter smithii and/or the individual reports bloating. Fermentable carbohydrates (i.e., sugars in dairy, fruits, vegetables) should remain low as the aforementioned bacteria will act upon oligosaccharides, disaccharides, monosaccharides, and polyols synthesizing gas and bloating.1(270) Finally, introduction of antibacterial agents such as berberine, citrus seed extract, and garlic can help control overgrowth.2(390) If fungal markers are high, oil of oregano and caprylic acid can be helpful.2(390)
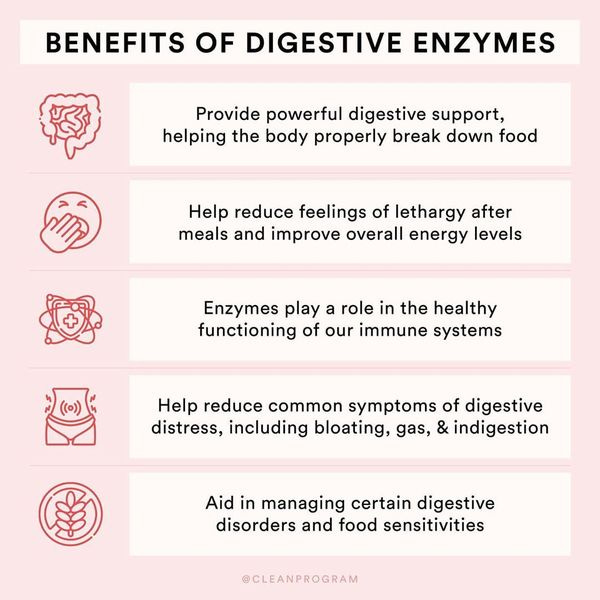
The second phase of FRP includes replacing digestive enzymes, if determined as deficient. Biomarkers which can help identify sub-optimal digestive enzyme production can emanate from comprehensive stool samples; such tests can provide insights on the digestion, and absorption, of macronutrients. If, for example, stool samples reveal high concentration fecal fat, such suggests steatorrhea, although the cause is not elucidated (maldigestion or malabsorption).2(422) If triglycerides are high, such would indicate incomplete fat hydrolysis/maldigestion likely due to insufficient pancreatic lipase production.2(422) If long-chain fatty acid stool concentrations are high, malabsorption is suspected since said fatty acids are known to be readily absorbed in a properly functioning gut.2(422) Ultimately, said findings would indicate the use of oral pancreatic enzyme supplementation, and betaine hydrochloride (if poor stomach acidity is detected).2(455)
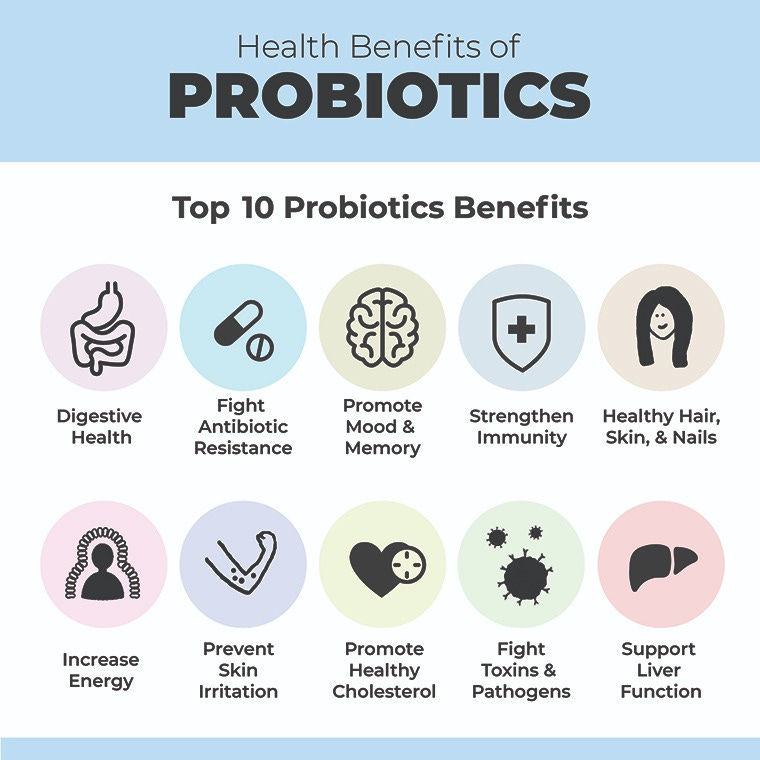
The third phase of FRP would include re-introduction of beneficial microbes when and where indicated. Probiotics are microorganisms which share a harmonious/symbiotic relationship with the gastrointestinal tract. Said microorganisms facilitate the prevention of diseases (i.e., inflammatory bowel disease, antibiotic associated diarrhea), modulate immune system function, and enhance epithelial barrier function.6 Hence, probiotics are necessary members of the gastrointestinal tract. When considering repopulating the gut with beneficial microbes, Lord et al2(440,454-455) suggested implementation of favorable microbes to help control toxin-producing species, toxin buildup (i.e., measured by high glucuronidase; an enzyme which makes the body reabsorb toxins), and general dysbiosis using L. acidophilus, L salvarius, L. plantarum, L. casei, and Saccharomyces boulardii.
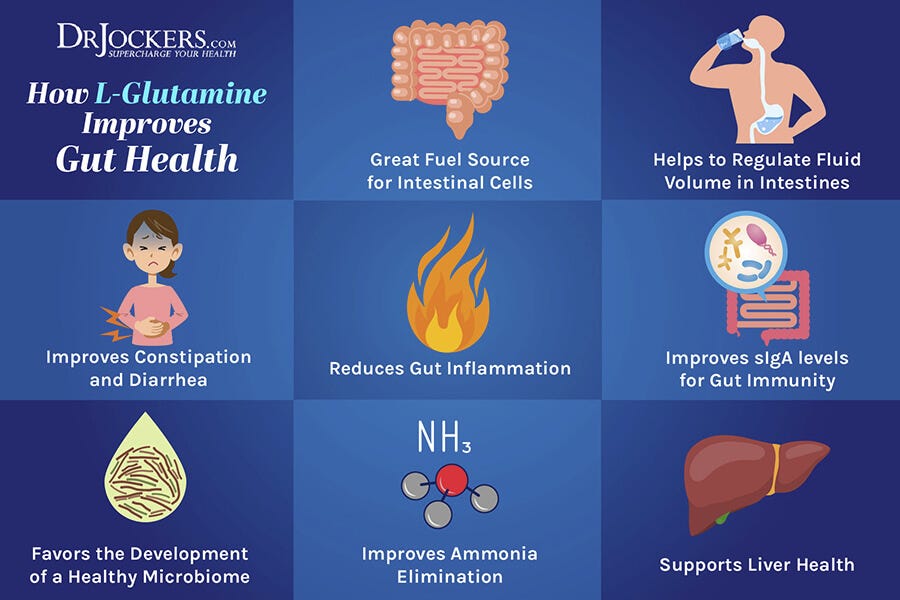
The fourth phase of FRP includes repair of the intestinal tract. If intestinal permeability is present, which can be measured by the lactulose/mannitol test covered in this author’s previous posts, implementation of glutamine can provide an energy source to facilitate/expedite the repair of intestinal tissue. Essential fatty acids such as eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) can also help remodel cell membranes along the intestinal wall in addition to supplementation of zinc, vitamin A/C/E, folic acid, pantothenic acid (B5), and free form amino acids to support cell growth and protection.2(455) Said phase might also be an appropriate period to include supplementation of micronutrients determined as deficient. For example, if a blood chemistry/organic acids lab indicate low magnesium/selenium/methylmalonate (a measure of B12) and high orotate (a measure of low arginine), consuming foods rich in said nutrients and concomitant supplementation of the same might be indicated, especially in the presence of severe deficiencies.
In conclusion, IBS is a frequently diagnosed gastrointestinal disorder accounting for an excess of 2 million family physician visits in 2002 within the United States. Furthermore, IBS is a multifactorial and complex disorder often characterized by abdominal pain, discomfort, altered bowel habits, as well as bloating and gas. When such symptoms are present, additional testing to confirm underlying drivers of IBS is indicated to include blood, urine, and stool analysis when and where available. Ultimately, such information produces a foundation of actionable knowledge from which a nutritionist can base nutritional and supplemental interventions for IBS.
References
1. Kohlstadt I. Advancing Medicine with Food and Nutrients. 2nd ed. London, NY: CRC Press; 2012.
2. Lord RS, Bralley JA. Laboratory Evaluations for Integrative and Functional Medicine. Duluth, GA: Genova Diagnostics; 2012.
3. Hawrelak JA, Myers SP. The causes of intestinal dysbiosis: A review. Alt Med Rev. 2004;9(2):180-197. http://archive.foundationalmedicinereview.com/publications/9/2/180.pdf. Accessed March 2, 2020.
4. Wexler HM. Bacteroides: The good, the bad, and the nitty gritty. Clin Microbiol Rev. 2007;20(4):593-621. doi:10.1128/CMR.00008-07.
5. Ghoshal U, Shulkla R, Srivastava, et al. Irritable bowel syndrome, particularly the constipation-predominant form involves an increase in Methanobrevibacter smithii, which is associated with higher methane production. Gut and Liver. 2016;10(6):932-938. doi: 10.5009/gnl15588.
6. Khalighi AR, Khalighi MR, Behdani R, et al. Evaluating the efficacy of probiotic treatments in patients with small intestinal bacterial overgrowth (SIBO)- A pilot study. Indian J Med Res. 2014;140(5):604-608. http://www.ijmr.org.in/temp/IndianJMedRes1405604-481902_132310.pdf. Accessed March 2, 2020.
-Michael McIsaac